Beyond the yuck factor: what works, what doesn’t and what we still don’t know about poo transplants
Doctors are trialling faecal transplants to treat a range of gut and other conditions, write Nadeem O. Kaakoush and Hazel Mitchell.
Doctors are trialling faecal transplants to treat a range of gut and other conditions, write Nadeem O. Kaakoush and Hazel Mitchell.

OPINION: The intriguing, yet somewhat malodorous, topic of poo transplants is in the news. A study published yesterday found poo transplants are better at treating a particular type of diarrhoea than an antibiotic or placebo (a fake or dummy treatment).
The study collated and analysed the results from earlier studies in how effective poo transplants were in treating diarrhoea caused by the bacterium Clostridium difficile.
Researchers have been interested in alternative treatments for this condition due to the rise in resistance to standard treatments (including antibiotics). So this type of diarrhoea has quickly developed into a more life-threatening disease.
The study findings are in line with recent European advice strongly encouraging setting up centres specialising in poo transplants to treat C. difficile diarrhoea.
Despite the apparent success of poo transplants for this particular condition, there is still much we don’t know about this therapy. It’s important to figure out how long the effects last, and which bugs in the poo transplant help us cure disease and which don’t.
Poo transplants (or “faecal microbiota transplantation”) involve transferring poo from a healthy donor to a sick recipient. The collective community of bugs and compounds (the gut microbiota) in the donor’s poo is then believed to establish itself in the recipient’s gut.
The scientific consensus is poo transplants work if the recipient’s gut microbiota is “restored”. The most consistent measure of this has been an increase in the diversity of the community of organisms in the recipient’s gut. By encouraging a more diverse and beneficial community of organisms in the gut, the idea is that this allows the recipient to resist being overwhelmed by the “bad” bugs.
Before donating their poo, donors’ poo and their blood is screened for many infectious agents such as C. difficile, HIV and viral hepatitis (A, B and C). This is to make sure a donation doesn’t transfer pathogens (disease causing microorganisms) by accident.
The screened donor poo is then delivered to the recipient in a number of ways.
Delivery methods from above involve recipients swallowing a poo capsule (or “crapsule”) containing frozen poo. Alternatively, a diluted sample can be delivered through a plastic tube inserted into the nose down to the stomach or small bowel (nasogastric intubation).
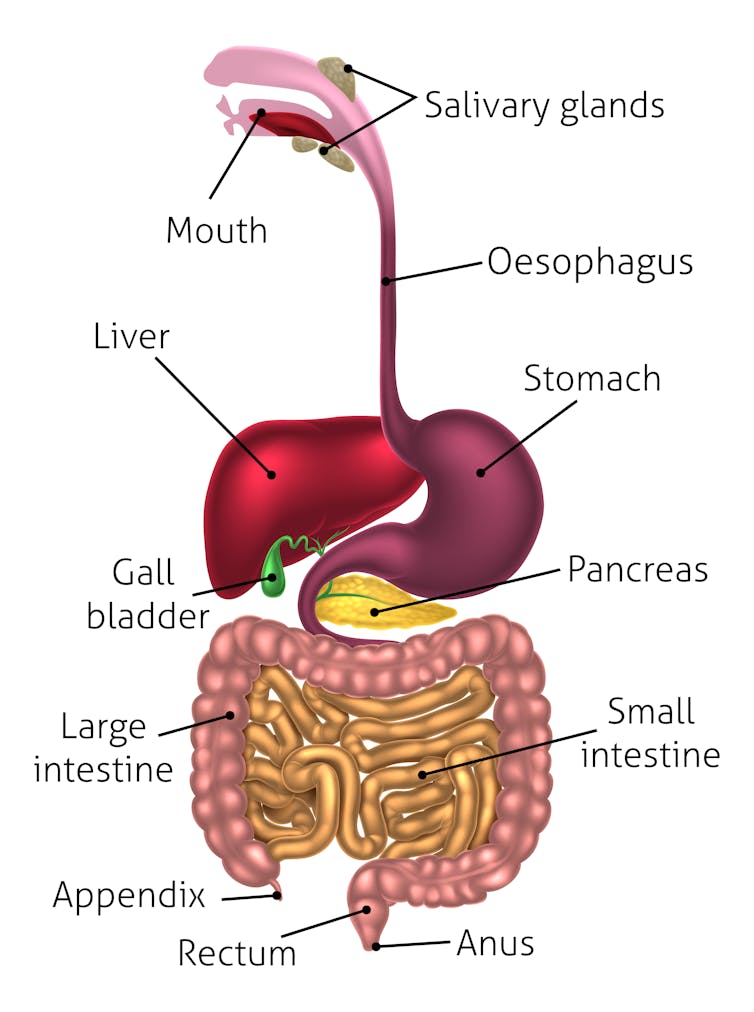
Samples can also be delivered from below via colonoscopy, where a tube is inserted into the rectum and goes deep into the gut to the caecum (just above the appendix). Or recipients can have an enema, where fluid is infused through the rectum.
Poo transplants made their way into the medical literature a long time ago with the first successful result in 1958. Interest in poo transplants was ignited in 1989, in Australia, when various conditions including irritable bowel syndrome responded to therapy.
However, it was not until 2013 that the first controlled trial for C. difficile diarrhoea was carried out, which showed the treatment was better than antibiotics and placebo.
The trial was stopped early as the ethics committee considered it unethical to withhold this therapy from the control group. The research out today backs these findings.
There is also evidence that poo transplants may be beneficial for patients suffering from the gut conditions colitis and Crohn’s disease, a range of infectious or inflammatory liver conditions, and in eliminating antibiotic-resistant bacteria from recipients’ guts.
Preliminary studies also suggest benefit for coeliac disease (in a single person), irritable bowel syndrome (in mice), and for bowel and behavioural symptoms in children with autism spectrum disorders (this was a small study).
Some studies have not shown a benefit from poo transplants for some of the above conditions. For example, a study in 2015 that looked at the effectiveness of poo transplants in patients with ulcerative colitis (a type of chronic inflammatory bowel disease) did not find a significant benefit.
The likely reason poo transplants do not work for all people is because we are still some way away from a defined, consistent form of this therapy.
Future research will focus on which bugs lead to poo transplants not working. For instance, work by our group suggests the Fusobacterium group of bacteria is one to watch. And other studies suggest certain viruses that infect bacteria (bacteriophages) could play a key role in the effectiveness of poo transplants.
We also need to keep in mind both “good” and “bad” bugs may differ according to the disease.
Poo transplants can also lead to generally mild side-effects like wind, cramps and constipation. There are also reports of patients with inflammatory bowel diseases worsening after therapy but this was found to be marginal and it’s unclear if the therapy itself was the cause.
There are many aspects of poo transplants we need to study in more detail. We still don’t know:
All these factors also depend on the type of medical condition being treated.
For instance, a recent meta-analysis (analysis of a combination of earlier studies) shows ulcerative colitis symptoms improved with a greater number of transplants and when these transplants were given through a lower route.
We now need to conduct other well-designed controlled studies on the conditions mentioned above as well as other conditions, and update treatment guidelines for the medical community.
While there is much we don’t know about poo transplants, there is growing evidence they can work for certain conditions.
If you’re thinking about this type of treatment for yourself or a loved one, consult your GP and gastroenterologist, and only use practitioners experienced in this therapy.
Nadeem O. Kaakoush, Senior research fellow, UNSW and Hazel Mitchell, Professor, School of Biotechnology and Biomolecular Sciences, UNSW
This article was originally published on The Conversation. Read the original article.
This article was co-authored by Professor Thomas J. Borody, founder and medical director of the Centre for Digestive Diseases (CDD). He declares a grant to CDD from Australia Research LLC, for research into faecal microbiota transplantation, and he has filed patents in this field (numbers US5443826 and US6645530).